Germicidal UV: a tradeoff between disinfection and indoor smog
The answer will vary for different times and locations, and here we illustrate how to think about it
If transmission is airborne, we must clean the air
We now know that airborne transmission is the only important way in which COVID-19 spreads. I.e., infected people exhale aerosols that contain the SARS-CoV-2 virus (although the aerosols are mostly saliva or respiratory fluid —the liquid that lines your lungs, trachea etc.). Those aerosols float in the air, and accumulate indoors. When others inhale those floating aerosols, they can become infected.
This knowledge has led to proposals of various methods to remove or “kill” the virus that is floating in indoor air, so that we can reduce transmission of COVID-19. The easiest and most recommended methods include ventilation with outdoor air and filtration (e.g. with Corsi-Rosenthal boxes or HEPA filters).
Germicidal UV
Ultraviolet light (“UV”) has been known since at least the 1930s to be an effective disinfectant of airborne pathogens, first with measles and later with tuberculosis. When used in this way, we refer to it as “germicidal UV” or GUV. In 1947 Westinghouse had a “marketing campaign urging a [GUV] Sterilamp in every American home, not to mention supermarket, bus station, bowling alley, school, and baseball stadium,” as a way to reduce the incidence of disease (Ep. 13 here). At the time, infectious disease and public health researchers were of the opinion that no important disease was airborne, so the idea was abandoned. After the demonstration (and widespread acceptance) in 1962 that tuberculosis is airborne, GUV has been used in some medical facilities, but has remained a “niche” technique in medical research and practice.
With the COVID-19 pandemic, there has been much more interest on GUV, with experts calling for much wider application. The denials and continuing confusion from Public Health officials to say clearly that COVID-19 is airborne, however, have slowed the widespread application of this and other air cleaning techniques.
What are the current GUV methods?
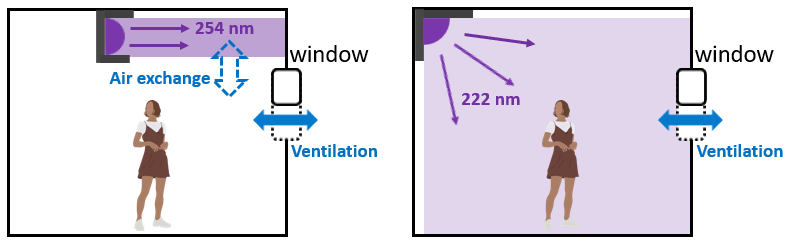
At present there are two main ways in which GUV can be applied, which use different types of UV lamps, shown in the schematic below. The traditional method uses mercury lamps that emit light at 254 nm. Since that light is damaging to human skin and eyes, it is typically installed near the ceiling of the room. That way the UV light can disinfect the air that naturally goes up and down in the room, without shining directly on people. Over the last decade lamps that produce light at 222 nm (sometimes referred to as “far UVC”) have been developed. They can also “kill” the airborne pathogens. But because they are absorbed so quickly by the outer layer of dead skin on our bodies, some scientists argue that they are safe to shine on a whole room, including the on people in it. Although not everyone agrees, this is already being done in many places. At present the 254 nm lamps are about 20 times cheaper than the 222 nm lights, so they dominate actual applications, but the balance may shift in the future
Could GUV create indoor smog? But wait, what is smog?
Smog is a colloquial name for photochemical pollution. As it name indicates, it needs photons of UV light (typically from the sun) and chemical ingredients (“primary pollutants”). The ingredients, such as volatile organic compounds (VOCs), are often the result of human activities. With those ingredients, chemical reactions form “secondary” pollutants including particulate matter (PM) and ozone (O3).
We associate smog with outdoor air, where both ingredients are present. In indoor air, there are plenty of chemicals, in fact more than in outdoor air. The figure below is a recent summary in the scientific literature comparing how many VOCs are present in indoor vs outdoor air. The typical home (US and Europe) has ~300 μg/m3, while outdoor air is typically lower except in very polluted megacities. In fact, the typical home has levels of VOCs comparable to very polluted outdoor air in Mexico City.
So we have plenty of chemical ingredients indoors for photochemical smog. But indoor air has much less UV light than outdoors, and therefore photochemistry indoors tends to be very slow. But if we add GUV, we are adding the missing ingredient that smog needs to get going. Is it enough light to make a difference? We’ll see below.
Does smog really kill people?
This was easy to see for very extreme events such as the Great smog of London of 1952. But most of the time, you need very careful statistics to pull out an association. For outdoor PM this was most clearly done in the Harvard six-city study of 1993, as shown in the graph below. Mortality clearly increased with fine particle levels. As undeniable as the increased mortality may appear, it was not obvious to the inhabitants of those cities. And when the six-city study was published, it was met by denials and lawsuits from polluting industries, and it took a long time for the fact that PM pollution kills a millions of people to be accepted.
Now we know that PM air pollution is one of the largest causes of preventable deaths (several million people a year worldwide). Ozone is thought to kill several hundred thousand people a year.
Studying GUV smog
The pandemic brought focus of many scientific disciplines onto specific scientific areas. Atmospheric scientists like myself got involved in virus transmission research. When we encountered proposals about wide application of GUV, we asked “but what about the indoor smog that GUV will create, is that important?” I assumed that some colleague would point out a scientific paper from the 1970s where this had been shown to be unimportant. But if such a paper exists, we have not found it. To our surprise, the fact that GUV could lead to non-negligible chemistry seemed to be news for much of the GUV community. We were told by some that people breathing GUV-disinfected air were not dropping dead or developing obvious ailments, and therefore this chemistry must be unimportant.
The fact that GUV-exposed people don’t quickly develop obvious health problems is reassuring. But it does not rule out the possibility of smaller effects that could e.g. accumulate over time and still be non-negligible, as in the case of the size-city study discussed above. There is a urgent need to quantify the risks due to GUV-created smog, and to compare them to the benefits provided by disinfection.
Given this vacuum of knowledge, Dr. Zhe Peng, Prof. Shelly Miller and myself decided to try get a first answer quickly using our computer model. Prof. Miller is an expert on GUV with decades of experience, and Dr. Peng and I had been working on chemistry initiated by UV light for most of the last decade. We were focused on a very different application (creating smog on purpose to better understand its sources), but the chemistry is the same. We took from the scientific literature (a) the typical composition of indoor air; (b) typical ventilation conditions; (c) typical GUV applications; (d) the chemical mechanisms of the chemistry created by UV light; and (e) the key chemistry of smog, and combined these five pieces to study this question.
How much GUV-induced smog is formed?
This week we have published a peer-reviewed paper in Environ. Sci. Tech. Letters (that was available as a preprint since Aug. 2022) where we present the results of this initial investigation. I will focus here on the big picture for a broad audience; scientists interested in the details should read the paper.
The results are not black nor white. GUV-induced smog is not so small that we can completely ignore it. But is is also not so bad that we should stop using GUV lights, especially in high risk environments. It is a case that calls for a risk/benefit analysis for different types of situations.
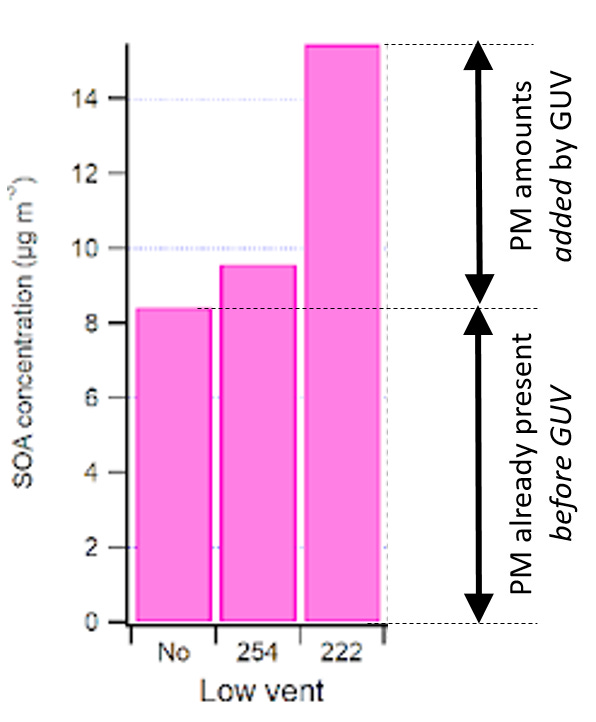
Why do we say that? Although there are several types of pollutants formed by GUV light that merit consideration, such as ozone (which is formed directly from 222 nm light), oxidized VOCs, and ultrafine particles, I will focus on the pollutant that’s best understood in terms of its health effects: PM. Below if the graph from the paper that shows the SOA (a type of PM) that is present indoors for different low-ventilation scenarios. What we call “low-ventilation” in the paper is typical of many homes and schools. We focus on low-ventilation here because that is when GUV would be most useful for disinfection (as we show in the paper). At high ventilation rates, the ventilation is already removing a lot of the virus, so the additional benefit of GUV is smaller. Then there is less incentive for the expense and inconvenience of adding GUV lights
The key result is the difference between the left bar (no GUV) and the middle and right bars (GUV at 254 and 222 nm, respectively). We see that the indoor smog due to GUV254 increases PM by about 1 μg/m3, and GUV222 by about 7 μg/m3.
Those are micrograms per cubic meter. It sounds pretty small. Is everyone going to have a respiratory crisis when exposed to this increased PM? Definitely not. But is it negligible? Unfortunately not.
What is the order-of-magnitude of the PM health impact from GUV smog?
We know that increased PM has important health effects, such as increased deaths from ischemic heart disease, stroke, chronic obstructive pulmonary disease, acute lower respiratory illness, and lung cancer. We need to estimate the impact of GUV PM quantitatively. We all agree that if the answer is 0, we can install GUV in without (this) worry. If the answer is higher, we need to compare it to the deaths avoided by reducing airborne diseases. So what is our best estimate? As a basis for the calculation, we will assume that GUV systems were installed in 1% of the indoor spaces in the US.
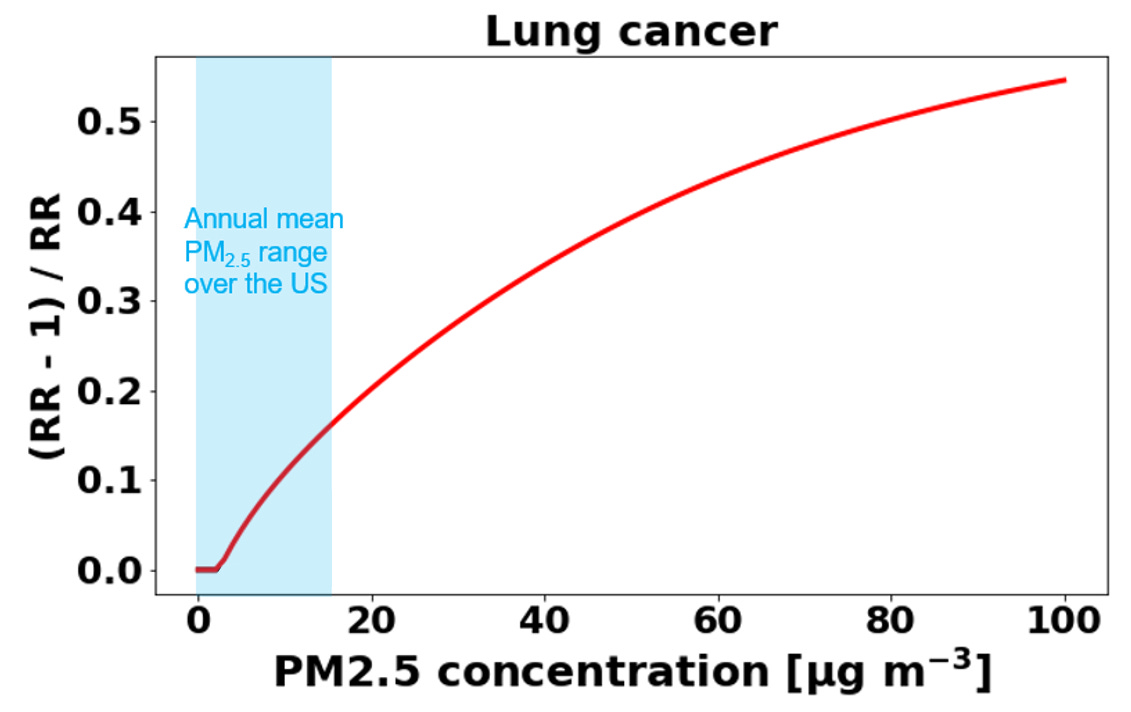
We turn to the best methods of current science. Based on epidemiological studies, they produce estimates of how much the deaths increase for a certain cause as PM increases. Below we show the curve for lung cancer deaths. How do we use that curve?
The X axis is the PM concentration to which people are exposed.
The Y axis is the increase in the lung cancer death rate due to increased PM. Deaths from lung cancer in the US are about 132,000 per year.
An example: if PM increased all over the US, such that the relative increase on the Y axis was 0.01 units, then the deaths from lung cancer would increase by 0.01 x 132,000 = 1320 additional deaths.
Now that we understand that, what is the impact of GUV? Starting with a typical PM concentration in the US (7.5 μg/m3, middle of the blue area in the graph), an increase of 1-7 μg/m3 results in an increase in relative risk of 0.012-0.075. For our case above where UV disinfection is deployed into 1% of US indoor spaces, lung cancer deaths increase by 16-99 per year. Now, that is only lung cancer. When we add the deaths from the other impacts of PM, we get a total estimate of 193-1100 extra deaths per year.
So what is the risk / benefit calculation for GUV?
We know that COVID-19 continues to kill about 300 people a day in the US as of this writing, or about 100,000 people per year. CDC estimates that the flu leads to 12,000-52,000 deaths per year in the US. Clearly reducing transmission of those airborne pathogens should reduce the death burden. Let’s assume that GUV was installed in 1% of indoor spaces in the US, potentially avoiding 1% of those deaths, or about 1300 deaths per year (we focus here on deaths for simplicity, although there are many other important impacts on health such as long COVID).
Assuming most of those spaces where GUV was installed had low ventilation, the estimated deaths from increased indoor PM of 193-1100 are smaller to comparable than the reduction in deaths from airborne infections of ~1300.
Under medium and high ventilation, the increased PM is much smaller. However, the benefit of disinfection is also significantly smaller, as ventilation is doing a lot of the work.
This tradeoff will also vary in time. If SARS-CoV-3 or a new flu virus spread in a few years and is as bad as SARS-CoV-2 with similar policies, we could have e.g. 460,000 deaths per year, so the avoided deaths by implementing disinfection would be greater (4600) in this case.
This is just an “order-of-magnitude” estimate. There are several complexities that are not incorporated. E.g. an infected person can transmit to other people that are not present in the GUV space. Then the reduced transmission has a benefit that acts beyond the GUV PM disbenefit. The timescale of the PM effects can be longer, so this comparison is most appropriate for longer term periods of GUV use. The PM effects are from a model, and the real world effects may be smaller… or larger.
Do other air cleaning techniques create smog?
Ventilation with clean outdoor air, when possible, and filtration, are very effective at both removing the virus and decreasing indoor pollution, especially PM which is the most dangerous pollution component. Thus in my opinion, and that of much of the scientific community, they should be preferred when they can put into practice. However, it is not always practical to increase ventilation and filtration enough. In particular, it is difficult to get very high air cleaning rates in high risk environments with those techniques.
The only other technique that experts have tentatively recommended is GUV, which has the tradeoff we just discussed.
There are many other techniques trying to use various chemical methods to “kill” the virus, such as plasmas, ions, photocatalysis, chemical sprayers and foggers, and others. All of those are known to create indoor smog, and some of them do not even work to reduce the risk of infection. Unfortunately, billions of dollars have been spent during the pandemic installing some of these “air cleaners,” e.g. in schools. Attempts to remove them are met with stonewalling and denials from school officials and others. So the results discussed below should not be viewed as an endorsement of other air cleaners based in chemistry. In our case we are focusing on studying GUV because it is extremely effective for disinfection, so it is most urgent to understand the extent of the smog problem.
What’s next?
Many research groups, including ours, are working to further clarify the issues discussed here. We can expect rapid progress, but on a scientific timescale of months to a few years.
If you have comments or suggestions, please post them below. An advantage of Substack (vs. Twitter) is that I can actually update the post to correct mistakes or to incorporate useful suggestions.






This was really interesting. I am thinking bout various work environments of people who had to show up during the lockdowns and thinking about how to both protect them and factor in the co-morbities they may bring to the table. That research is likely farther off.
Also, as I work with meat production plants with high levels of ammonia, chlorine and organic particulate matter...how do those higher levels interact with GUV and change the smog calculations
I've been following you for quite some time on Twitter, and I love your effort on promoting the airborne nature of this virus, and the ways to mitigate transmission.
Our government (The Netherlands) has _decreased_ the ventilation requirements for restaurants, bars and clubs (I think by a factor of 5!) last year, in the midst of the pandemic, and they are proud of it...
I hope they will one day listen to you.